Sharper View of Eye Surgery
Introduction
Imagine needing to perform a surgery looking through the tunnel of a microscope. You need to manipulate your surgical tools within the space of a pea or less, and there’s no tactile feedback. You also need to use both feet to control certain features of your equipment. It’s not a task that you’d want to perform on a live patient for the first time, is it?
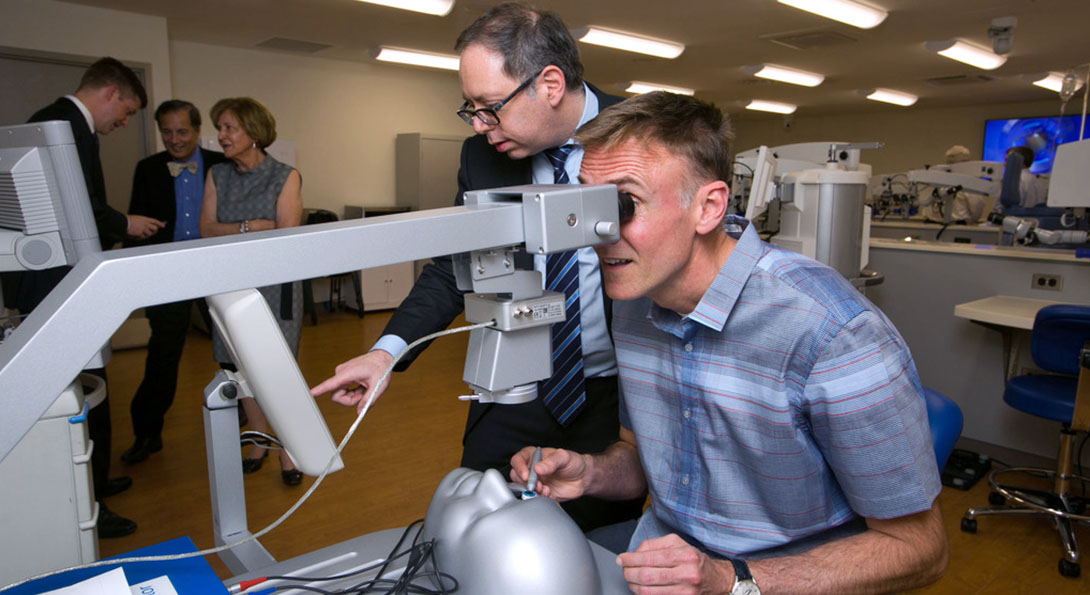
This need to hone fine skills before treating patients underlies the creation of the Cless Family Ophthalmologic Training and Simulation Center housed in the Eye and Ear Infirmary. The lab lets ophthalmology residents, fellows and surgeons perfect eye surgery techniques in a simulated surgical setting. The Cless Family Lab has been in use since 2015, but was officially dedicated in June when the department hosted a ribbon cutting ceremony.
“Surgeons need to simultaneously use their hands, feet and eyes in a highly coordinated fashion for most surgeries,” said Mark Rosenblatt, professor and head of ophthalmology and visual sciences in the College of Medicine. “Being able to practice in a dedicated eye surgery simulation environment means they can easily practice both routine and new surgeries so that the risk for complications is significantly reduced when they operate on patients.”
The lab includes nine surgical simulation stations. Each station has two surgical microscopes that look down on an operating field. One is for the fellow or resident practicing – the other allows an instructor or partner to observe the operation.
Trainees and surgeons can operate on a partially disposable plastic eye, a pig or human eye, or a highly advanced computerized plastic eye that senses the surgeons tools inside the eye and projects a realistic simulated video image of a human eye undergoing surgery back through the microscope in real time 3-D.
Most of the stations also come with several pre-programmed modules or a defined curriculum that allow surgeons to practice specific surgeries. On the simulated eye, Rosenblatt chooses a cataract surgery module and gets to work breaking up a virtual cataract and vacuuming up the debris. He uses the same exact machine, hooked up to the surgical station, that he uses in the operating room to pulverize and remove a cataract.
“It’s tremendously hard to mimic eye surgery outside the operating room, but the Cless Family Lab gets very, very close,” said Jose de la Cruz, assistant professor of ophthalmology and visual sciences in the College of Medicine. “The lab is really an advanced teaching tool, and we have built training curricula around the use of the lab. But students can always come to the lab on their own time to practice outside of formal classes.”
All the microscopes can project their field of view onto four large flat-screen monitors around the room so that others in the lab can watch along. The video can also be transmitted outside the lab to other simulation labs, to conferences or to physicians in other countries. Just as the video from the lab can be shared outside UIC, the screens can also receive video feeds from other labs or operating rooms so that surgeons can practice along with surgeons in another state or country. All the video feeds can also be recorded and stored for later viewing.
“All the tools used in the wet lab are exactly the same as those tools the surgeon would use in the operating room,” said de la Cruz. The surgical simulation lab also lets surgeons get the feel for using new surgical instruments. The Cless Family Lab has already hosted a regional course training senior surgeons new forms of less invasive corneal transplantation.
The lab, which has multiple philanthropic funders, is named after the Cless family. Gerhard Cless first came to know UIC in 1995 when he was referred for treatment for a macular hole. Since 2000, The Cless Family Foundation has funded an array of projects and needs for the department including vision research and education programs, the acquisition of advanced microscopy, recruitment of faculty, clinical studies and support for a retina fellowship. Prior gifts also established the Gerhard Cless Endowed Lecture, the Cless Best of the Best Award and the Cless Family Professorship in Ophthalmology.